Benign Prostatic Hyperplasia – BPH
BPH – Benign Prostatic Hyperplasia (Enlarged Prostate)
Most men – if they live long enough – suffer from BPH (Benign Prostatic Hyperplasia). BPH is the swelling or enlargement of the prostate which occurs naturally in men as they age.
How does BPH occur?
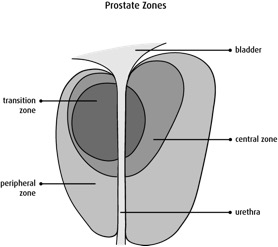
The innermost layer of the prostate – the transitional zone – gradually begins to swell in middle aged men and is a normal part of the ageing process. An enlarged prostate begins to cause problems when it interferes with daily activities.
Why is BPH a problem?
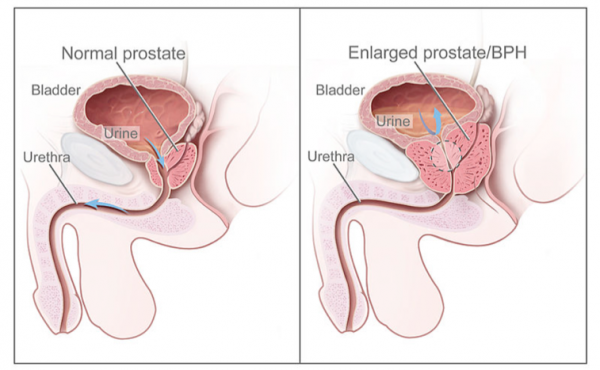
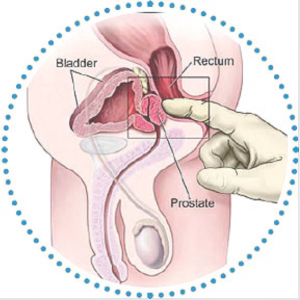
The prostate gland is situated between the bladder and the penis. The urethra – which transmits urine from the bladder and semen when we ejaculate – runs through the centre. An enlarged prostate can cause the following issues because of its location in the body:
- Difficulty urinating -BPH gradually compresses and narrows the urethra making urination slower and more difficult.
- Increased night time urination – when the prostate enlarges upwards it alters the shape of a valve at the bottom of our bladder. This valve is more affected when we are lying down making night time urination more frequent.
What Are The Symptoms of BPH?
- Slowness of urinary flow
- Frequent urination
- Difficulty urinating
- Night time urination
- Dribbling after urinating
- Urgency
What are uncommon symptoms of BPH?
If you are experiencing any of the below symptoms it is recommended that you visit your GP.
- Blood in the urine – should be checked with your GP but it can sometimes be caused by BPH.
- Pain on urination – likely to be due to infection or inflammation and needs to be investigated.
- Pain on ejaculation
- Frequent urination – This may be diabetes if associated with thirst and drinking a lot of fluids.
- Lower abdominal pains
If you think you may have BPH, the first thing to do is complete the International Prostate Symptom Score, or IPSS which is available here. Ideally print off your copy and bring it with you to your prostate check-up.
The total scored is divided into three categories.
| Total Score | Significance |
| 0-7 | Mild symptoms |
| 8-19 | Moderate symptoms |
| 20-35 | Severe symptoms |
 Mild Prostatic Symptoms
Mild Prostatic Symptoms
If you are experiencing mild prostatic symptoms, you can adopt some simple measures and repeat the score in one year:
- Reduce the amount that you drink before a particular activity where frequent urination would be a problem. Also, don’t drink within 2 hours of bedtime.
- After passing urine, go back to the toilet again after a few minutes to try to pass some more to ensure the bladder is emptied completely.
- Consider reducing or stopping caffeine (commonly found in tea, coffee and cola). Coffee is the worst.
- If urgency is a problem try some distraction techniques such as breathing exercises and mental tricks (for example, counting) to take your mind off the bladder.
- If frequency is a problem try retraining the bladder by holding on for as long as you can each time before passing urine. The bladder muscle can be trained to expand more in this way. Eventually, the bladder may be trained to hold on for longer each time before you need to go to the toilet.
- If you are a smoker then stopping smoking may significantly improve your symptoms, as nicotine directly irritates the bladder. This is not a myth.
 Moderate to severe symptoms.
Moderate to severe symptoms.
If you are experiencing moderate to severe symptoms – and score more 8 or more on the IPSS – you should get your prostate checked.
That can be done here with us in the Beacon, or you could go to your own GP. It helps if you print off your IPSS score and bring it with you.
While symptoms of BPH are most of the time caused by an enlarged prostate, there can be other reasons which need to be checked. A prostate check-up ideally involves the following:
- A prostate symptom questionnaire
- Physical examination by a doctor
- Urine and blood tests
- An ultrasound examination of your bladder
Find out more detail about what is involved here.
What happens next?
Your results will depend on what happens next which will be one of the following:
- Do nothing specific except the general measures advised for mild prostate symptoms.
- Your doctor may suggest medical treatment with tablets.
- You may be referred to a specialist called a urologist. This is usually because of more severe symptoms, a concern about prostate cancer, a bladder abnormality or just to get another opinion.
There are two types of medicines used for treating BPH. These are called:
- Alpha Blockers
- 5-alpha reductase inhibitors (5ARIs)
 Alpha Blockers
Alpha Blockers
With BPH the slowing of urine flow is caused by a combination of two problems:
- The physical swelling of the innermost layer of the prostate
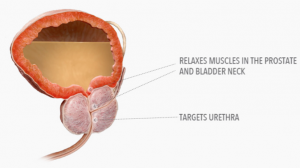
- The action of a type of muscle called smooth muscle within the gland, at the bottom of our bladders. When these smooth muscles over-tighten they can squeeze the urethra – the tube that we urinate through – and slow down the flow of urine.
Smooth muscle cannot be consciously told what to do by our brains, unlike our other muscles which do what they are told, such as move my thumb.
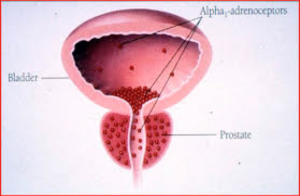
Alpha Blockers are medicines that relax smooth muscles and can be used to treat the symptoms of BPH.
Selective Alpha1 Blockers work specifically on prostate and bladder muscles. They mainly block the so called Alpha 1A receptors – found in the bladder and prostate – rather than the Alpha1B receptors found in the arteries therefore they don’t have they same, negative side effects as older Alpha blockers.
Alpha 1 blockers are taken once a day, and generally improve things within a week. They can be taken indefinitely and side effects are uncommon.
Side Effects of Alpha 1 Blockers
All these will go away if the drug is stopped, but most men are happy to continue with these drugs. Side effects can include:
- Dizziness
- Tiredness
- Runny nose
- Difficulty ejaculating
- Retrograde ejaculation – this can happen where a man experiences orgasm but no semen comes out.
There is a possible link with a disorder known as ‘floppy iris syndrome’, and it is advised that anyone taking an Alpha 1 blocker and needing eye surgery inform their surgeon they are taking the medicine.
The most commonly used alpha blockers are:
- Silodosin – arguably the most refined Alpha1 blocker. This Alpha1 blocker has been proven least likely to cause dizziness and unsteadiness often due to a sudden drop in blood pressure.
- Tamsulosin
- Afluzosin
The improvement noticed with an Alpha Blocker may eventually wear off, but most men will get many years of relief and improvement.
5-Alpha Reductase Inhibitors (5-ARI)
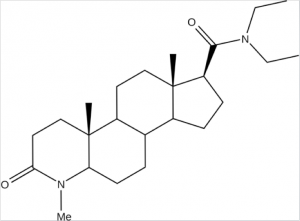
These drugs work by shrinking the prostate and letting urine flow easier by blocking the conversion of an inactive hormone called testosterone to its active form. This happens only inside the prostate, and doesn’t affect our hormones elsewhere. It is like shutting off its food supply, and the prostate slowly reduces in size. This is very gradual, and takes up to 6 months before the effect is noticed.
They are really only suitable for men with moderately enlarged prostates. They also lower the blood levels of an important enzyme called PSA, which is produced by the prostate, and measuring the blood level of this is one of the ways that risk of prostate cancer is assessed.
There are two main 5-ARIs:
- Dutaseride
- Finaseride
They are taken once a day, and can be used indefinitely.
Side Effects of 5-Alpha Reductase Inhibitors (5-ARI)
Similar to the Alpha1 blockers, all side-effects should go away if the drug is stopped. If you have severe liver disease you should not take a 5-ARI.
- Loss of interest in sex
- Erectile difficulty
- Problem with ejaculation
- Swollen feet (rare)
There are concerns that 5-ARIs could be of harm to a pregnant woman, it is advisable not to donate blood if taking one, in case the blood is given to a pregnant woman.
Combination drug treatment for BPH
In theory, taking a combination of an Alpha Blocker and a 5-ARI drug should give us the best of both worlds – a fairly quick improvement of symptoms and a longer term reduction in the size of the prostate. However, this combination is best suited for men with moderately enlarged prostates. This makes sense, as small prostates will not benefit from size reduction. Very large prostates may be beyond medical treatment and usually need surgery.
A tablet that combines the alpha blocker Tamsulosin with the 5-ARI Dutasteride has been available for some years. Side effects are the same as those for the individual drugs.
Surgical treatment for BPH
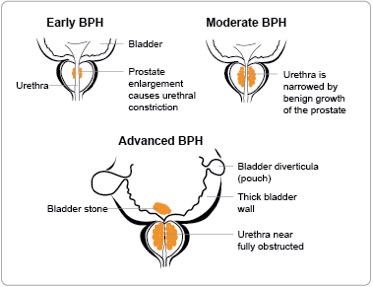
Surgical treatment for BPH has been performed for over a century, with newer techniques and instruments being developed. Most surgical techniques involve removing the inner part of the gland only, and leaving the outer sections. This is enough to allow us urinate freely.
There are many reasons why we may consider surgery for BPH. They include:
- Failed medical management. This could be because of unacceptable side effects, not enough improvement, or gradual loss of effectiveness of the treatment taken.
- More severe BPH, usually with higher IPSS score.
- Men with very large prostates.
- Acute urinary retention, especially if it recurs. When this happens we suddenly find it impossible to pass water, and it is a medical emergency. We will need to have a tube called a catheter passed up the penis into the bladder.
- Inability to empty the bladder. Here the bladder cannot fully empty itself, and gradually gets bigger and bigger. Eventually it can lose the ability to push the urine out.
- When there is evidence that BPH is causing kidney problems.
- Some of us may prefer to have surgery, and get it over with, as opposed to ongoing medication.
TURP can be described as getting a re-bore of the prostate, rather like the old fashioned apple corer, where only the centre part is removed and the rest left alone. Since it is the innermost layer of our prostate – called the transitional zone – that swells up and blocks the flow of urine, it makes sense just to remove this part.
How it is done?
TURP is only done in a hospital, with either a full general or a spinal anaesthesia. Your urologist will insert a resectoscope, a thin metal wire with a light, a camera and a loop at the end in through the penis. It goes up the urethra – the tube we pee through. He will view it on a monitor. An electrical current heats the loop, which cuts away the centre of the prostate.
Towards the end of the procedure a catheter, a thin flexible tube, is used to irrigate fluid into the bladder and remove all the cut sections of tissue. The operation takes about one hour. The catheter is left in temporarily. Normally, 24-48 hours after the op the catheter is removed, and you can go home. Most physical activities can be gradually resumed within 4 weeks, and there should be little pain.
What happens after?
Most urologists advise us to rest for one week, but walking around the house and garden is usually OK. You should find urinating much easier than before, but there will be some blood in the urine for a couple of weeks. It is also normal to have slight irritation and some urinary frequency because your bladder and urethra have been irritated during the op.
You will need to discuss with your urologist when it is safe to return to work.
Advantages of TUR
- 85% experience a significant improvement in symptoms
- Only 10% will need a second op – about 2% per year.
- Improvement is nearly immediate.
Problems of TUR
- The majority of men who have TUR are not able to ejaculate normally having sex, and suffer from ‘retrograde ejaculation’, where semen in ejaculated upwards into the bladder. However, the sensation of orgasm is not affected.
- Urinary incontinence happens to 2%. Mostly it is better in one month, but in some men it persists.
- The urethra – the tube we pee through – can be damaged, and symptoms similar to BPH can recur. This thankfully is fairly easy to treat, but with a minor op.
- Erectile dysfunction affects 5-10%, but can usually be successfully treated with medicine.
Here a specific laser beam vaporises rather than cuts away the centre of the prostate, and there is less blood loss than with traditional TUR. It can be done as a day case procedure, and takes roughly one hour.
The light from the KTP laser is absorbed by oxyhaemoglobin, which is in our blood, especially in red tissue with many blood vessels. There is a sharp increase in local temperature, which vaporizes the tissue but also coagulates it, so bleeding is minimal.
The bleeding rate for Greenlight treatment is less than 1% of the bleeding rate of conventional TURP – 0.21g/min v 20.1g/min. For this reason it is especially suited to men at risk from operative bleeding, which really means men on anti-clotting medication. Often it is risky to stop this for surgery, but with Greenlight it is unnecessary.
The overall success of Greenlight v TUR is similar, but hospital time and recuperation is shorter.
Advantages of Greenlight
- Possible discharge same day
- Normal activities resume in 3-4days
- Vigorous activities in 4-6 weeks
- No association with post-operative impotence
- Retrograde ejaculation may be less likely
Disadvantages
- It takes slightly longer to perform than a standard TURP
- It is not so effective on very large glands.
- No tissue is available for analysis to determine if prostate cancer is present.
- Discomfort or pain on passing urine is more common after a laser prostatectomy than after a TURP. This may last a week.
- Sometimes prostatic tissue may be passed after the operation, which could block passing urine.
- Complications can occur, although these are rare, and can follow inappropriate firing of the laser into the bladder and damaging the tissue in that area.
This could be considered as a ‘mini TURP’. It is also known as a ‘Bladder Neck Incision’. Under anaesthetic an instrument is passed up the penis to the upper part of the prostate, and two small cuts are made into the muscle there, relieving the urinary blockage, instead of removing tissue from the prostate as done for TURP. This will then open the bladder neck and prostatic urethra creating a wider channel through which you pass urine.
Why choose this?
- If you are at higher risk for complications from surgery and anesthetic, including men with serious health problems. TUIP involves less blood loss and can be done more quickly than TURP. The chance of side-effects following a TUIP are lower than that following a TURP
- For men with smaller prostates
- Less risk of retrograde ejaculation.
- Shorter operation time – less than 30 minutes.
What to expect afterwards.
TUIP is a much less invasive procedure than transurethral resection of the prostate (TURP). You are able to go home sooner after surgery. You may not be able to urinate and may need to have a catheter to drain your bladder. For most men, this lasts for a week or less.
How Well It Works
Symptoms improve after TUIP in about 8 out of 10 men. Men notice about a 73% improvement, but men who have TUIP are more likely to need a second surgery.
Risks
The possible risks of transurethral incision of the prostate (TUIP) include the following:
- Retrograde ejaculation, in which semen flows backward into the bladder, occurs in about 15%.
- Incontinence occurs in less than 1 out of 100 men.
- The need for a blood transfusion during surgery, although rare, is possible.
- For about 10 % a second operation is needed after 15 years.
Transurethral needle ablation
A surgeon uses high-frequency radio waves to cause thermal injury to the prostate.
Transurethral needle ablation is a relatively new procedure that uses needles to deliver interstitial low-level radio frequency energy to produce a temperature above 100 degrees C and subsequently cause prostatic cell tissue necrosis.
The procedure duration averages approximately 30-45 minutes.
TUNA can be performed under local anesthesia, IV sedation or transperineal prostate block. Therefore, TUNA does not require an additional hospital stay and is generally performed as an outpatient procedure.
The most common intra-operative complication reported is a burning sensation, which can be significant to cause the termination of the procedure in 1% of patients. However, this can be managed by a prostatic nerve block prior to beginning the procedure.
Like many of the other minimally invasive procedures, TUNA avoids significant intra-operative bleeding by heat coagulation. The overall incidence of peri- and post-operative complications following TUNA is ~25%, a rate that is significantly lower than TURP.
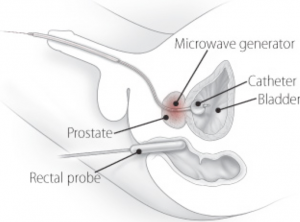
Transurethral microwave thermotherapy (TUMT)
Transurethral microwave thermotherapy is a minimally invasive surgical treatment which uses a device to apply heat to the prostatic tissue causing necrosis and relief of bladder outlet obstruction. While the improvements in some outcomes following TUMT have not quite reached those associated with TURP, significant improvements in urinary symptoms have been reported for long time periods. Overall, it is still unclear as to the long term effectiveness in the relief of lower urinary symptoms after treatment with TUMT. One of the major advantages of TUMT is that it can be performed in a single 1-hour session as an outpatient procedure without any general or spinal anesthesia.
It is not routinely available and is still regarded as experimental.
Botulinum Toxin injection of Prostate
Botulinum Toxin is a chemical that is now extensively used in medicine, which temporarily paralyzes muscles. In theory it should help BPH, but in practice it is not so effective.
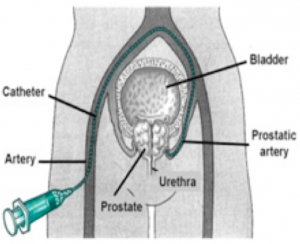
Embolisation of prostatic artery
This surgical technique is performed by radiologists, not by urologists. The artery going to the prostate is blocked, cutting off its blood supply and causing it to shrink.
This procedure is similar to getting a cardiac catheterisation, where a wire is inserted into the artery in the groin to the heart. It is only available in a few specialised centres in the UK, and is still regarded as experimental. The benefit of this is that it is a less invasive treatment than traditional surgery and may well become more common.
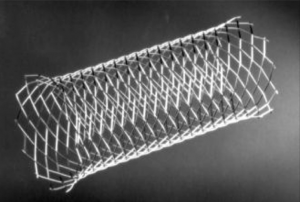
Prostatic urethral stent
This procedure uses a small mesh cylinder called a prostatic urethral stent, which is typically made of titanium. The doctor inserts the stent through the penis and, after positioning it in the narrowed area of the urethra, releases it to widen the channel, relieving pressure from the prostate tissue and allowing for easier urination. This quick procedure requires only local or spinal anesthesia, involves no loss of blood, and is often done in an outpatient surgical center.
Prostatic urethral stents aren’t for everyone. They are most often used in elderly men who have severe prostate enlargement and whose overall health is so poor that surgery would be risky. In many cases, urinary obstruction gradually returns because of a process called hyperplastic epithelial reaction, in which prostate tissue protrudes through the mesh and causes renewed blockage. There’s rarely a complete re-blockage of urinary flow, but additional procedures may be required in some cases.
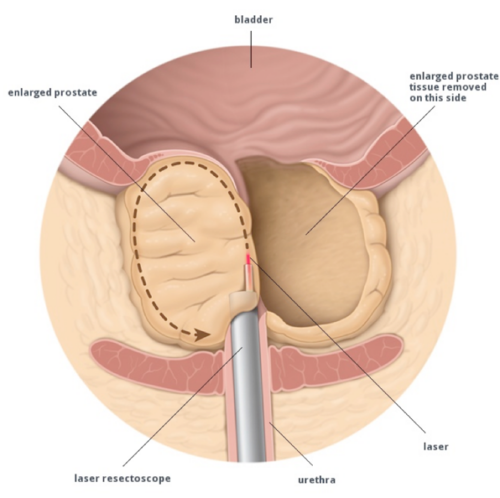 Holmium Laser Enucleation of the Prostate (HoLEP)
Holmium Laser Enucleation of the Prostate (HoLEP)
This is a newer technique where a specialised Holmium laser is used to remove the central sections of the prostate. It has some advantages over traditional TUR in that it can be done on larger prostates. There is also less blood loss.
It is a complex technique, needing expensive equipment, and is not universally available.
Who is it suitable for?
HoLEP can be performed on men of any age with urinary outflow obstruction caused by an enlarged prostate. It is particularly indicated in men with large prostates (over 60mls in size) and can possibly be used for men on medications to thin the blood such as warfarin, aspirin or clopidogrel.
What are the advantages of HoLEP?- There is no upper size limit of prostate that can be treated – traditionally men with prostates over 100ml in size needed major open surgery.
- There is often less bleeding than after a TURP.
- Discharge is often quicker than after TURP at 1-2 days.
- The chance of recurrence requiring further surgery is very low.
- Unlike TUR and Greenlight laser operations, large quantities of prostate tissue are sent for pathological analysis.
- The PSA generally drops to very low levels after HoLEP operations.
What are the disadvantages of HoLEP?
The procedure takes slightly longer than a TURP and requires specialist training. It is available only in some specialised centres.