Prostatitis
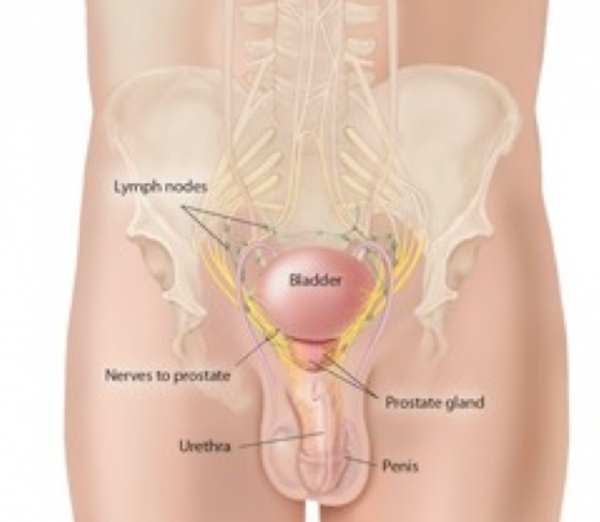
Prostate problems become more common in men over the age of 50. Common prostate problems include:
- BPH (Benign Prostatic Hyperplasia) – Enlarged prostate
- Prostatitis – inflammation of the prostate
- Prostate Cancer
What is Prostatitis?
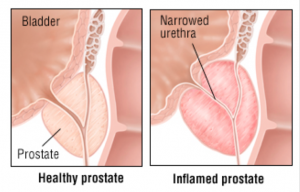
A word ending with ‘itis’ means that something is inflamed. So, prostatitis has to mean inflammation of the prostate. Or does it? There is no agreed definition of what prostatitis means. To attempt to clarify it, prostatitis is categorised into three types, each very different.
- Acute bacterial prostatitis.
- Chronic bacterial prostatitis.
- Chronic prostatitis – chronic pelvic pain syndrome.
- Chronic non-bacterial prostatitis, otherwise termed asymptomatic inflammatory prostatitis. Although included, this is best ignored, as there is doubt about whether it exists.
It usually affects a young man, who gets abruptly ill with high fever, pain passing urine, pain in the lower pelvis and in general feeling awful. There is a demonstrable infection of the urinary tract as evidenced by white blood cells and bacteria in the urine. It is always caused by bacteria – not a virus – and is treated by high dose antibiotics. Treatment is generally commenced in hospital, and continued at home once there is improvement.
This is rarer, usually affects middle aged men and is a type of infective prostatitis. It is caused by a persistent bacterial infection, coming on gradually, with low level pain in the pelvis, sometimes pain while urinating, and having to go to the toilet very often. A man with chronic bacterial prostatitis will usually have had recurring urine infections, as it is usually caused by the same type of bacteria that causes these urine infections. The bacteria can remain dormant in the prostate and therefore recurring infections can occur. It is not a sexually transmitted infection.
What are the signs & symptoms?
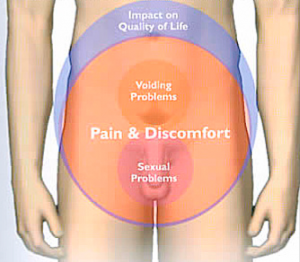
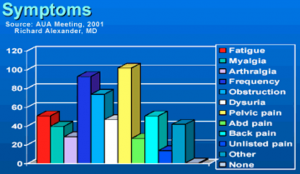
These tend to wax and wane. During a flare-up, there may be pain and discomfort, mainly at the base of the penis, around the anus, just above the pubic bone and/or in the lower back. Passing stools can be painful. There may be pain passing urine, going more frequently or an urgent desire to pass urine quickly.
All these are similar to the symptoms of acute bacterial prostatitis, but men with a flare-up of chronic bacterial prostatitis tend to be less ill than those with acute prostatitis. For example, a fever is uncommon and you are less likely to have general aches and pains.
Treatment
Chronic bacterial prostatitis usually responds to treatment with antibiotics. The choice depends on lab results, and usually they need to be taken for minimum 4 weeks.
This is loosely defined as pelvic pain without evidence of urinary tract infection, and lasting longer.
It can wax and wane. The pain can range from mild to severe. Pain may be felt the lower back and in the back passage, making sitting uncomfortable. It can also cause pain in the perineum (the area between the scrotum and the back passage), in our testicles, tip of the penis, in the pubic bone or sometimes in our bladder area.
The cause of this type of chronic prostatitis is not fully understood. Many theories have been put forward as to the cause. These include:
- infection of the prostate with a germ that has not yet been identified;
- nerve problems affecting the prostate;
- an autoimmune problem of the prostate gland (antibodies that we normally produce to fight infection may be attacking the cells of the prostate gland for some reason);
- Inflammation resulting from urine being forced backwards up into the prostate at the time of urination.
Stinging on urination, muscle aching, abdominal pain, constant burning pain in the penis, and urinary frequency may all be present. Constant tiredness is common. Almost all sufferers will be referred to a urologist for this very distressing condition.
To diagnose chronic prostatitis/chronic pelvic pain syndrome, a urologist must rule out all other possible causes of urinary symptoms, such as kidney stones, bladder disorders, and infections. Since many different conditions must be considered, the doctor may order a full range of tests, including ultrasound, blood tests, and tests of bladder function. Sometimes an MRI scan.
If all other possible causes of symptoms are ruled out, the urologist may then diagnose chronic prostatitis/chronic pelvic pain syndrome. To aid in understanding the symptoms and measuring the effects of treatment, the doctor may ask a series of questions from a standard questionnaire, the NIH-Chronic Prostatitis Symptom Index. Link here
If you are attending your GP or urologist about possible CPPS, it is useful to download and fill in this questionnaire and take it with you.
Treatments include:
- Antibiotics. Sometimes, even if no bacteria are found on testing, they can relieve the symptoms.
- Medications to relax the prostate muscles. These are called alpha-adrenergic blockers.
- Non-steroidal anti-inflammatory medication, such as ibuprofen.
- Acupuncture helps sometimes
- Relaxation techniques, usually under the advice of specialised physiotherapists, are increasingly being used.
How to cope with Chronic Pelvic Pain Syndrome
Your GP will probably refer you to a specialist urologist, and hopefully your symptoms will be relieved. Unfortunately, all too often no cause is found and no treatment may seem to work. If so, there are some other avenues:
- Referral to a specialised physiotherapist
- Acupuncture has had success with CPPS
- Formal stress reduction techniques
- Exercising more does seem to help
Referral to a specialised physiotherapist
Some physiotherapy clinics have developed an expertise in treating CPPS, using a number of complementing techniques. Your urologist could recommend one. The management plan recommended by physiotherapists is similar to this one.